Program Mission
The Physician Assistant Program at the University of Maryland Eastern Shore is dedicated to ensuring equal opportunities for all students, with an emphasis on supporting those from diverse backgrounds. Our mission is to empower students to deliver compassionate and competent care to patients in underserved and diverse communities locally, nationally, and globally.
Program Vision
The Physician Assistant Program at the University of Maryland Eastern Shore will become an innovative healthcare leader recognized for its excellence in PA education, research, and community service.
Program Goals and Effectiveness in Meeting Its Goals
* Benchmark- reference point used to assess the program’s performance in a specific area. If the program meets its benchmark, it indicates effectiveness in achieving its goals; if not, it highlights areas needing improvement.
- Survey benchmarks are >3.5 on a 5-point Likert scale.
- Survey strength benchmark- 4.5 or greater for three (3) consecutive years
- Survey area of needing improvement- Less than 3.5 for two (2) consecutive years
- UMES PA program will recruit, select, and retain diverse applicants who can complete the rigorous Master of Medical Science in Physician Assistant Studies (MMS-PAS) program.
- The UMES PA program is effective at recruiting and selecting diverse applicants, but can improve in the area of retention as illustrated with the Admissions/Orientation Survey, Student Diversity, and Attrition data.
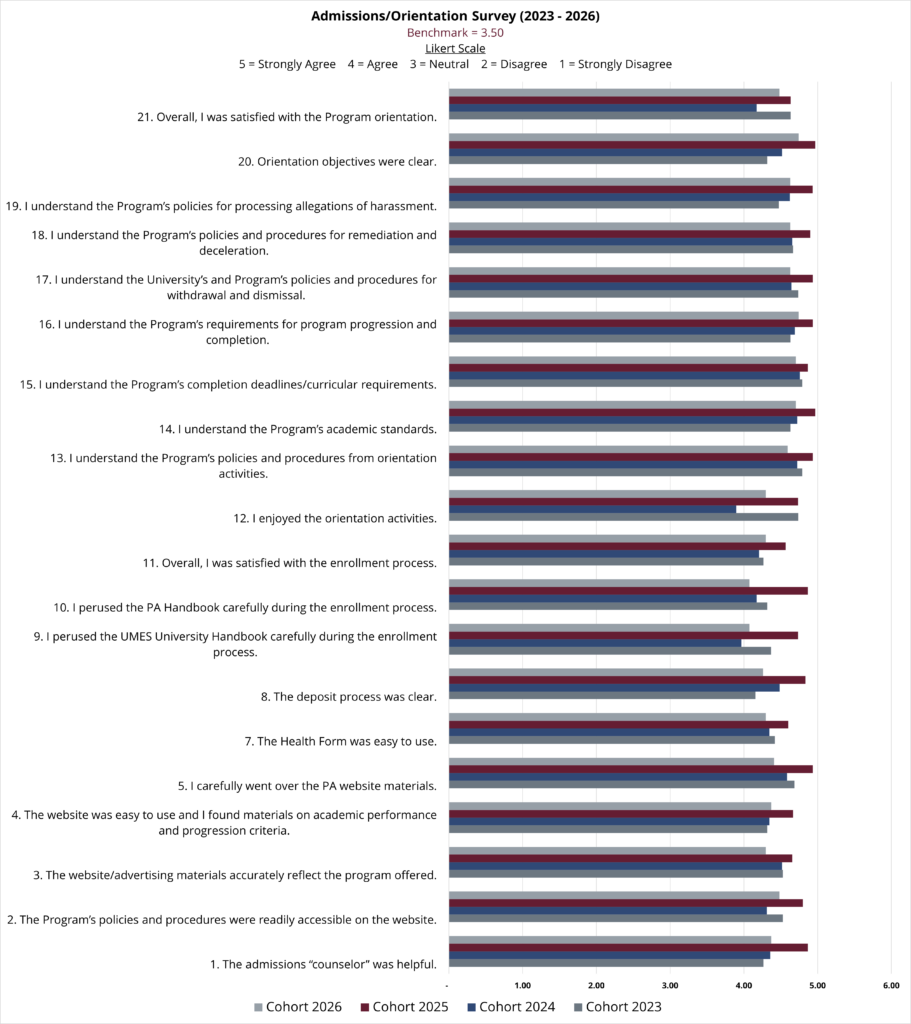
- The Admissions survey data highlights the superior admissions process. The program has exceeded its >3.5 benchmark since its inception.
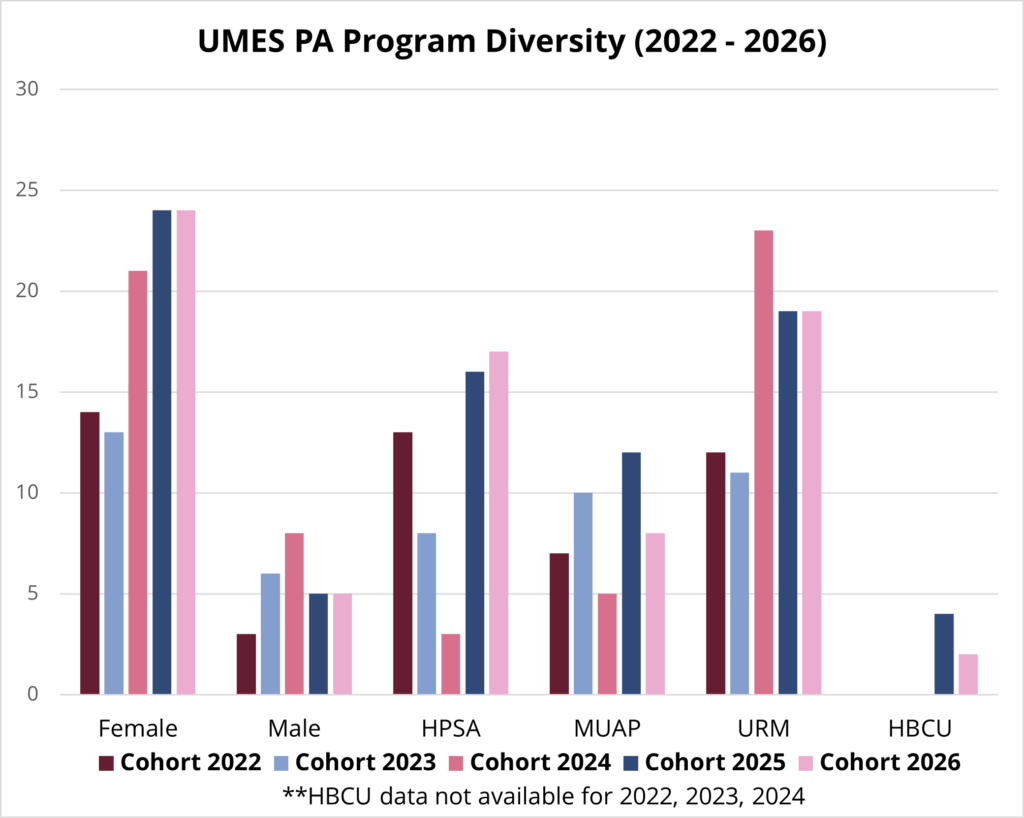
- The Student Diversity data highlights the the range of backgrounds represented within the program. The UMES PA program defines student diversity as students from underrepresented backgrounds e.g. underrepresented minorities in healthcare as defined by PAEA by the numbers report, individuals from health professional shortage areas (HRSA) and medically underserved areas/populations (MUA/P), those attending HBCUs, military veterans, and first-generation college graduates. Note: military veteran and first-generation college graduate data will be forth coming. The program has a 75% diversity benchmark. This benchmark was exceeded with each cohort except cohort 2023.
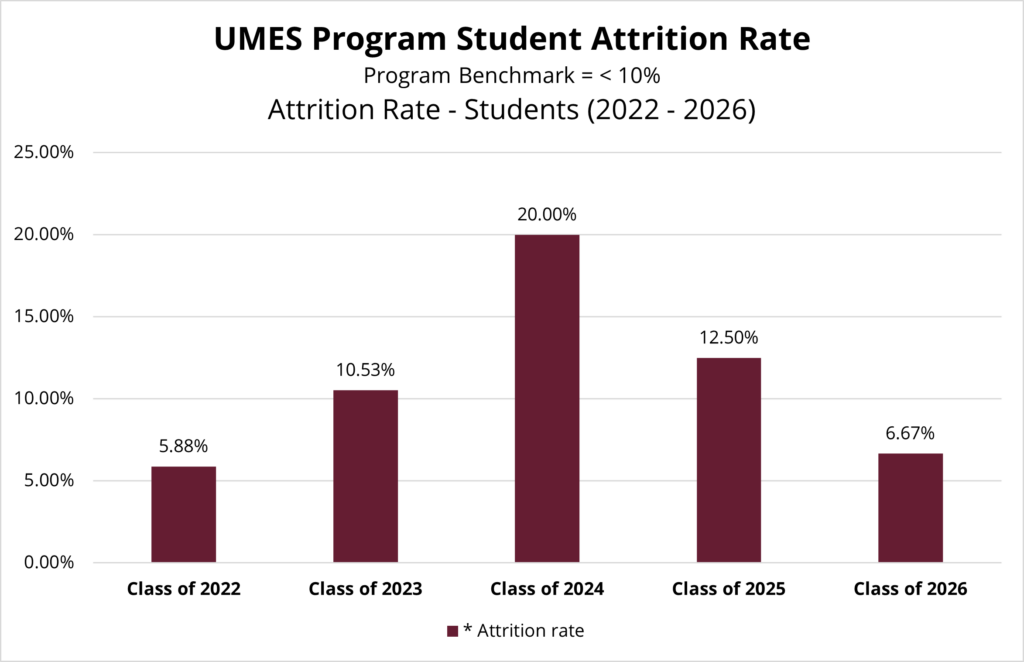
- The Attrition data highlights the UMES PA program’s ongoing efforts to retain diverse applicants. However, the program did not meet its benchmark of maintaining an attrition rate below 10% for the 2023, 2024, and 2025 cohorts. The data includes both students who have decelerated to a subsequent cohort and students who permanently left the program. The program is actively working to implement strategies to improve retention and achieve this important benchmark.
- The UMES PA program is effective at recruiting and selecting diverse applicants, but can improve in the area of retention as illustrated with the Admissions/Orientation Survey, Student Diversity, and Attrition data.
2. Prepare physician assistant students to demonstrate medical knowledge, clinical reasoning, clinical and technical skills, interpersonal skills, and professional behavior to provide high quality patient care.
- The UMES PA program is effective at achieving this goal as illustrated by the Exit Survey, Preceptor Evaluations of the Student, and PANCE First-Time Pass Rate data.
- The Exit Survey highlights graduates perception of their preparedness to demonstrate medical knowledge, clinical reasoning, clinical and technical skills, interpersonal skills, and professional behavior in order to provide high quality patient care. The program exceeded its >3.50 benchmark with Cohorts 2022 and 2023.
- The Preceptor Evaluation of the Student highlights the preceptors perception of UMES PA students’ ability to demonstrate medical knowledge, clinical reasoning, clinical and technical skills, interpersonal skills, and professional behavior in order to provide high quality patient care. The program exceeded its >3.50 benchmark with Cohorts 2022 and 2023. The preceptor evaluation scores for each student were averaged for each cohort.
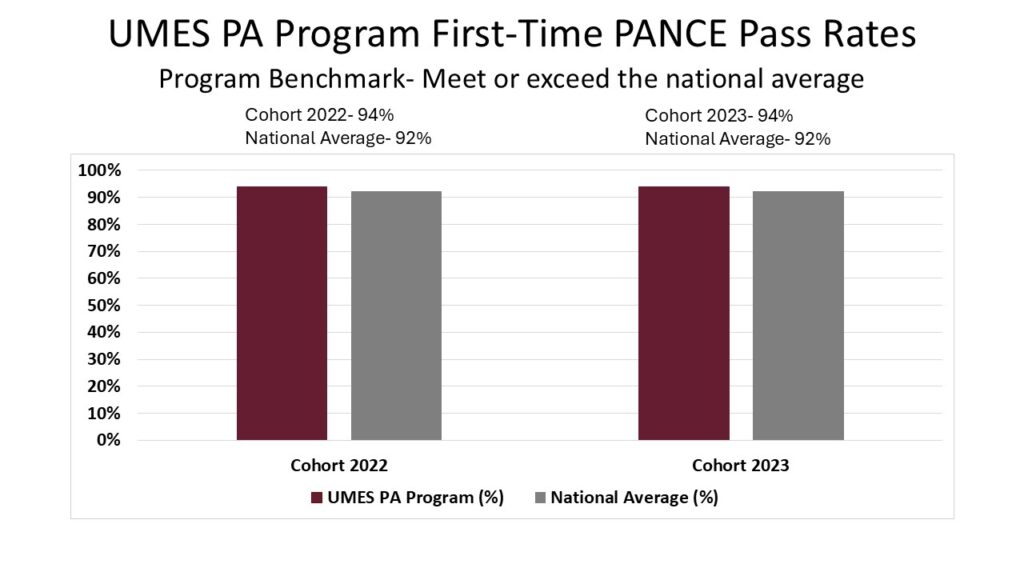
- The PANCE First-Time Pass Rate data highlights the UMES PA program graduates’ ability to demonstrate the medical knowledge and clinical reasoning necessary to provide high quality patient care. The program exceeded its benchmark for cohorts 2022 and 2023. Benchmark- Meet or exceed the national average.


3. Prepare graduates to master the skills necessary to become successful medical providers in interprofessional team-based practices.
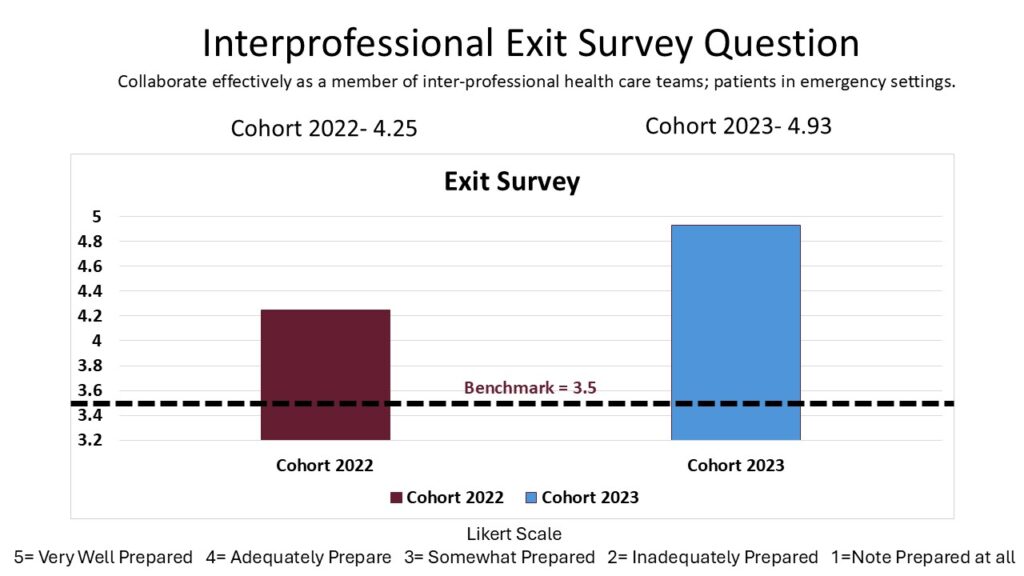
- The UMES PA Program is effective at meeting this goal as illustrated by the IPE survey and Exit Survey Question data.
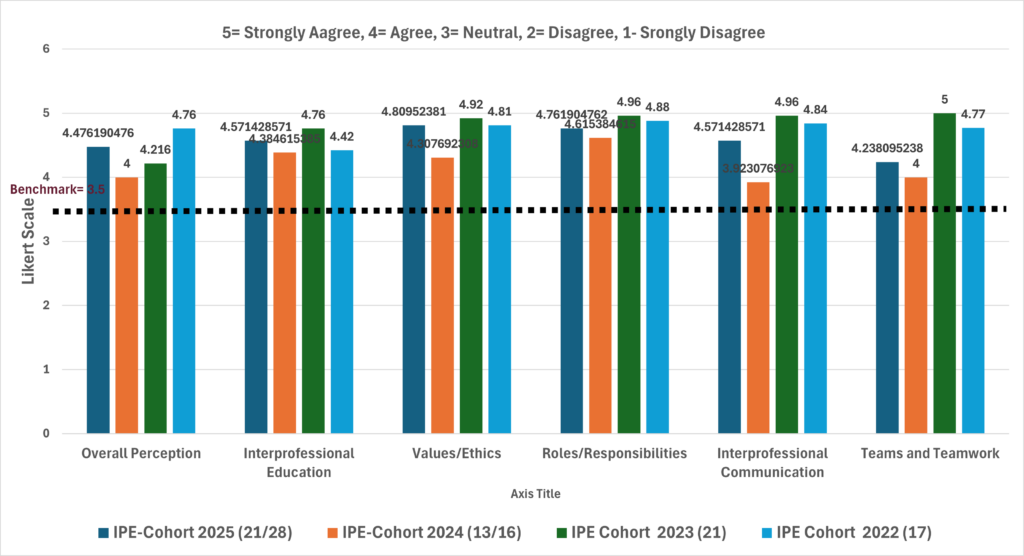
- The UMES PA Program participates in Interprofessional Education in a number of events with the other Health Profession students at Salisbury University and UMES. After the event, students are surveyed with a number of questions in the following categories: Overall Perception, Interprofessional Education, Values/Ethics, Roles/Responsibilities, Interprofessional Communication, and Teams and Teamwork. The program uses a benchmark of > 3.50. The program has exceeded this benchmark for all areas listed since the inception of the program.
- The Exit Survey highlights graduates perception of their preparedness to collaborate effectively as a member of the healthcare team. The program exceeded its >3.50 benchmark with Cohorts 2022 and 2023.
IPE Survey
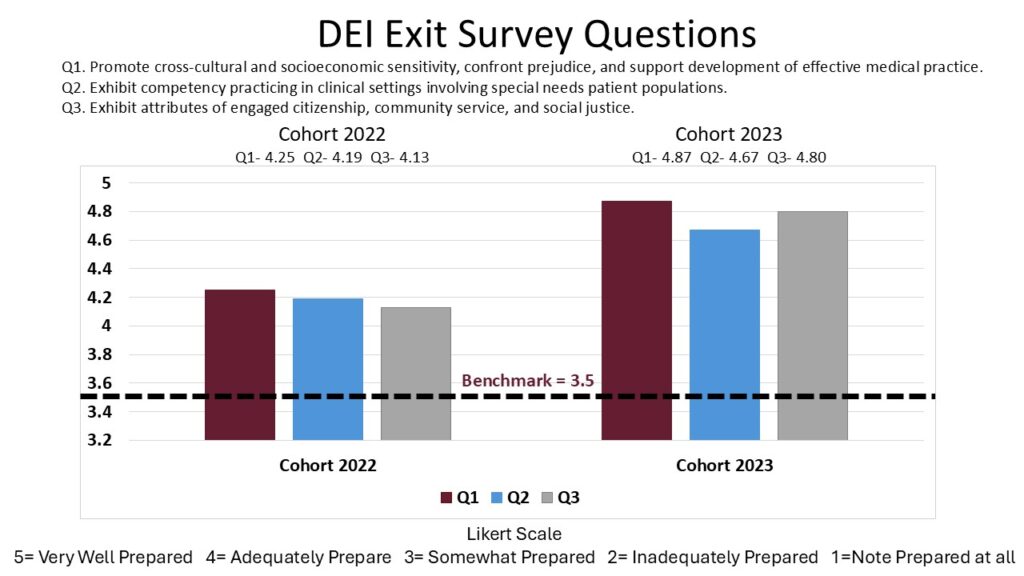
4. Cultivate a diverse, equitable, and inclusive (DEI) learning environment that prepares graduates to provide health care to underserved communities.
- This is a new goal developed by the program to create an environment where all individuals feel valued, respected, and supported, regardless of their backgrounds, identities, or circumstances.
- The program is working towards demonstrating effectiveness for this goal. The program has created a climate survey which will assess the perceptions, experiences, and attitudes of our faculty, staff, and students regarding the DEI culture within the program and the programs ability to prepare graduates to provide health care to underserved communities.
- The program currently has a DEI Exit Survey which provides some insight into the effectiveness of this goal. The program exceeded the >3.50 benchmark for both cohorts 2022 and 2023 illustrating students felt prepared in various areas of DEI to provide health care to patients. The exit survey will be updated in the future to align closely with the goal.
5. Foster an environment that inspires and supports student and faculty applied research initiatives related to the Physician Assistant profession.
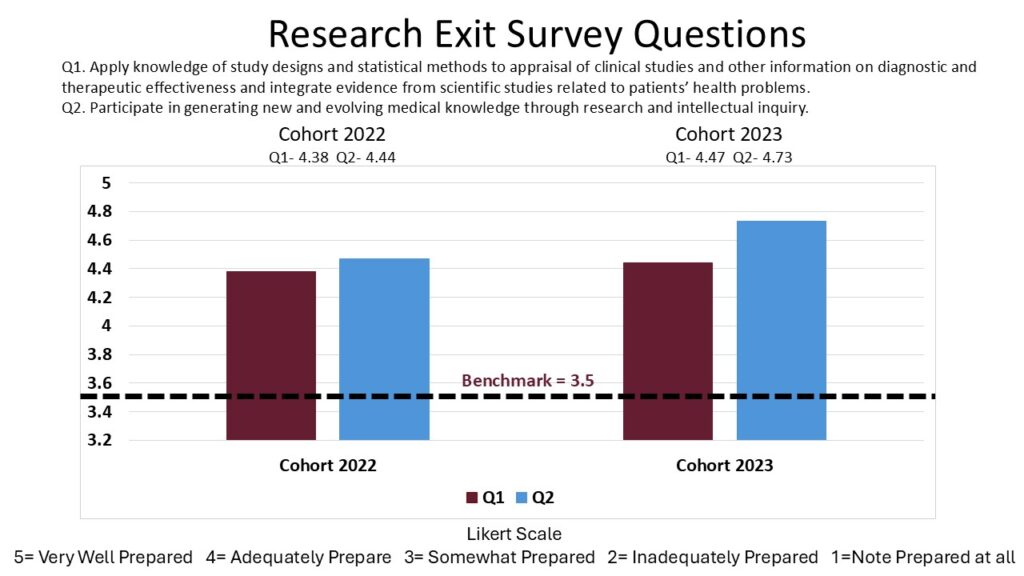
- The UMES PA program has been effective at achieving this goal as illustrated by the Research questions on the Exit Survey and Capstone Participation data.
- The Exit Survey highlights graduates perception of their preparedness to participate in research initiatives. The program exceeded its >3.50 benchmark with Cohorts 2022 and 2023.
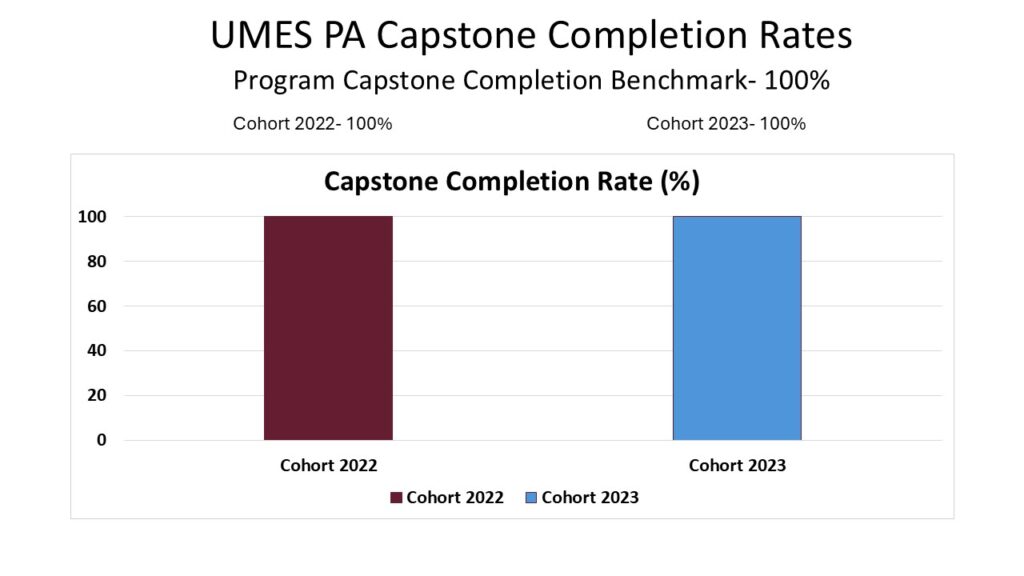
- The program requires all students to complete a capstone research project, beginning with a literature review to identify gaps in healthcare and formulate a research question to guide their work. Students then apply research findings to address real-world patient challenges, bridging the gap between academic theory and clinical practice. This process equips students with essential research skills and opens opportunities for presenting and publishing their findings. Students showcase their research at the Graduate School Research Symposium, and some have even presented at state conferences. The benchmark of 100% participation was met.
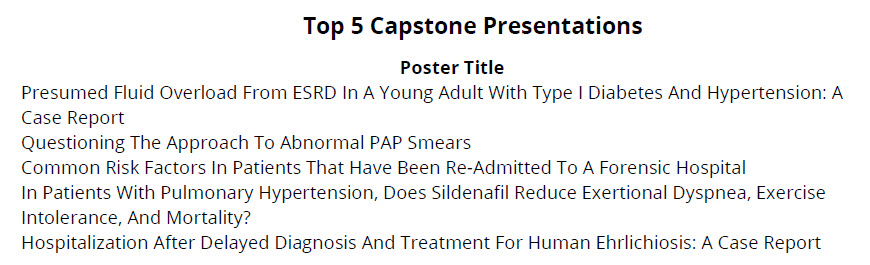
- Additionally, students transform their research into a poster presentation, shared with faculty, staff, and the community. Faculty evaluate the posters using a detailed rubric, assessing organization, visual design, and the student’s ability to address the research question, collect and analyze data, draw conclusions, and clearly articulate their knowledge of the topic. The 5 top-performing capstone projects from the inaugural cohort are highlighted below the capstone participation data.
- This goal was recently revised to include faculty. Faculty data points and benchmarks will be forth coming.